About Us
A Successful Thoracic Fluorescence-guided Surgery in General Hospital of Shenzhen University
A Successful Thoracic Fluorescence-guided Surgery in General Hospital of Shenzhen University
As the detection rate of pulmonary nodules increases constantly, a great deal of clinical intervention is needed accordingly. The thoracoscopic anatomical segmentectomy plays an increasingly important role in the treatment of this disease. The team lead by Dr. Xiaoming Zhang, Director of the Department of Thoracic & Cardio Surgery, General Hospital of Shenzhen University, recently performed a successful single port thoracoscopic segmentectomy by using Caring Medical’s fluorescence imaging system. The patient recovered well after operation and was discharged within a few days. Our NIR fluorescence imaging system was able to identify pulmonary segments, or even sub-segments without impeding the surgical field and this technology was proven to facilitate an accurate and complete segmental resection while preserving patients’ normal pulmonary function to the maximum extent.
The patient, 54 years old, CT found a 6mm a ground glass nodule in the outer basal segment of the left lower lobe (see Figure 1). Based on many years of clinical experience, Dr. Zhang considered that it was a typical mixed ground glass nodule with a very high probability of early lung cancer, so the surgical resection was recommended. Since the nodule was <2cm in diameter, in order to keep the patient’s normal pulmonary function maximally after completely removing the nodule, Dr. Zhang with his team decided to perform a single port thoracoscopic segmentectomy under the assistance of NIR fluorescence guidance.
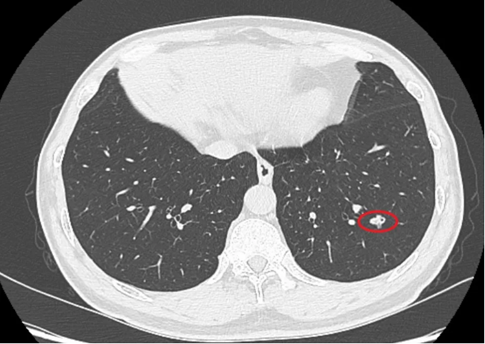
Figure 1. Nodules in the outer basal segment of the left lower lobe
During the fluorescence-guided thoracoscopic segmentectomy, Dr. Zhang first ligated the left pulmonary artery (See Figure 2) which provides blood supply to the targeted segment, and then he injected ICG via peripheral vein. It was a negative stain procedure as the targeted segment does not show any fluorescence without blood supply. This technology enables surgeons to identify the targeted segment intraoperatively in real time (See Figure 3) and thus can facilitate an accurate and complete segmental resection while preserving patients’ normal pulmonary function to the maximum extent.
The determination of pulmonary intersegmental plane is most critical in segmentectomy. Although the conventional method of “inflate and deflate” works fairly well, it takes about 15-20 minutes waiting for the lungs wholly collapse, which prolongs the operation time. NIR fluorescence technology can resolve this issue perfectly for the boundary between pulmonary segments shows up almost immediately after injection of ICG, therefore, the "fluorescence method" has proven advantages of being simple, fast, accurate and without affecting the surgical field of vision.
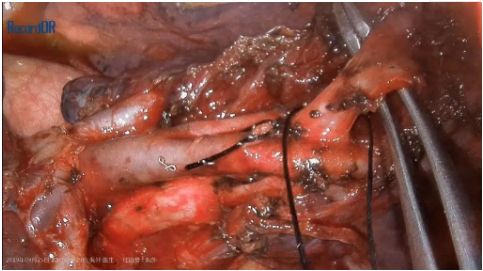
Figure 2. Dissociation and ligation of the artery in the outer basilar segment of the left lower lung

Figure 3. Intraoperative fluorescence imaging of pulmonary intersegmental plane
Indocyanine green (ICG) fluorescence imaging technology can facilitate precise localization and real time visualization of pulmonary segments. With the assistance of fluorescence guidance, the conventional single port thoracoscopic segmentectomy can truly conduct minimally invasive surgery (MIS) in an accurate and precise way. Therefore, this innovative technology will definitely benefit for the majority patients who suffer from early stage of pulmonary cancer.